Medicare Part D Direct & Indirect Remuneration
Payers who offer Medicare Part D plans may receive additional compensation after the point-of-sale. These funds are known as Direct & Indirect Remuneration (DIR), and account for growing levels of disparity between Part D gross and net drug costs. As DIR is primarily composed of manufacturer rebates on select drugs, the way rebates are allocated have unexpected effects on patient out-of-pocket (OOP) contributions and payer incentives.
Key Findings
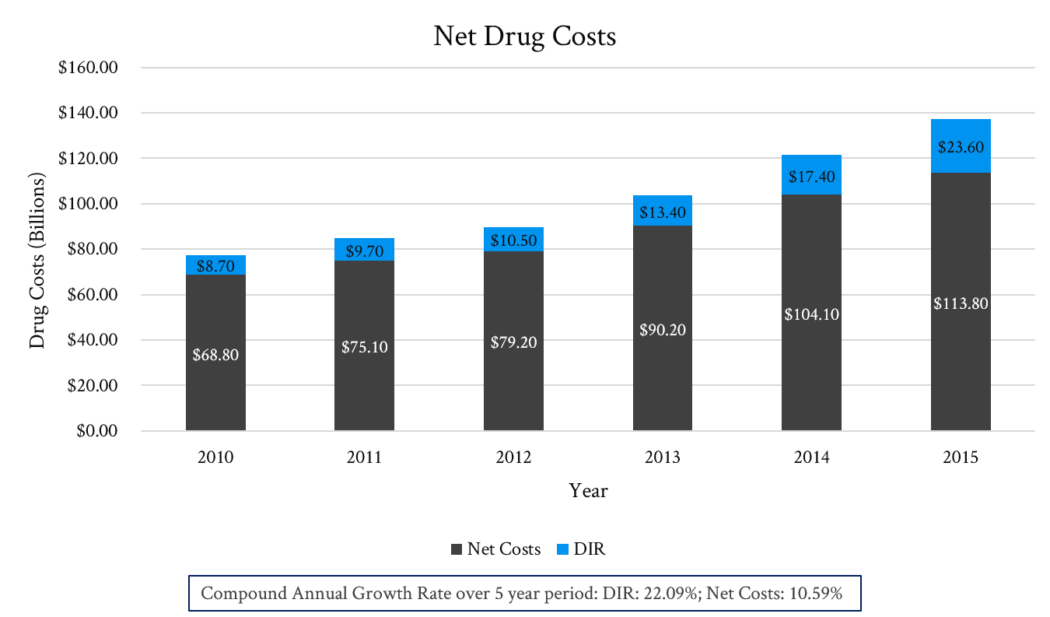
DIR as a percentage of gross drug costs has grown from 11.3% to 17.2% between 2010 – 2015. This change reflects the success of Part D payers in obtaining increasing levels of price concessions (rebates) for drugs in the Part D benefit. Total DIR reported by Part D plan sponsors has been growing dramatically in recent years (see Figure 1), with rebates growing at twice the rate of net drug costs between 2010 – 2015.
Implications for Life Science Manufacturers
Rebates paid by manufacturers are not applied to pharmacy network pricing which drives patient OOP amounts for individuals subject to coinsurance.
As such, patients do not benefit from lower OOP costs due to rebates and instead pay pharmacy network rates based on gross, not net price.
However, the manner in which DIR funds are allocated do serve to offset the premium rates Part D plan members pay monthly.
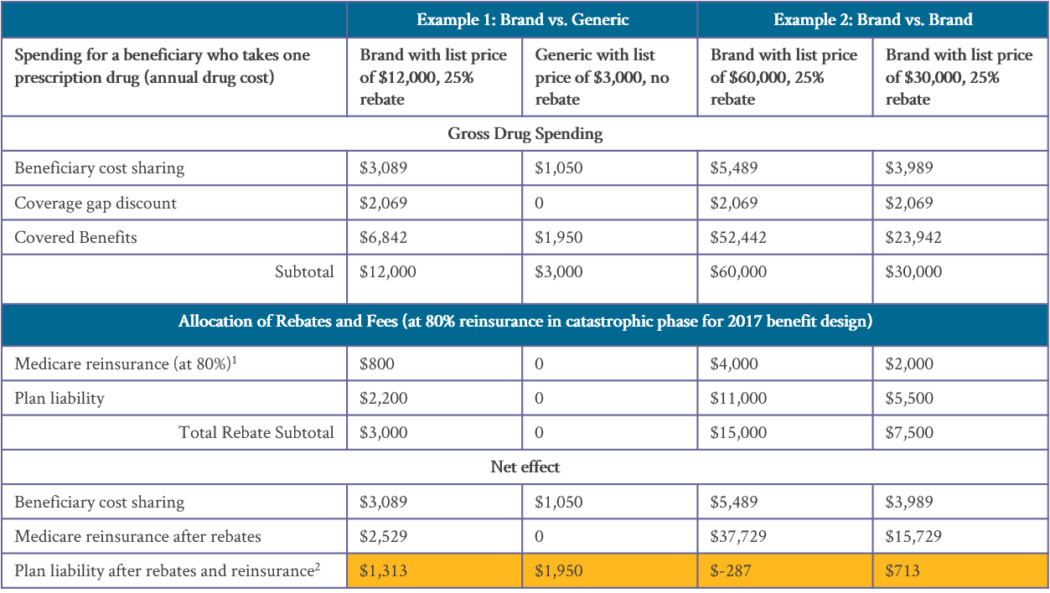
More importantly, the allocation of DIR funds may also provide an incentive for payers to prefer high list price / high rebate drugs over drugs with a lower list price (see Figure 2).
Conclusions / Action Steps
Part D members with coinsurance (particularly for those on specialty medications) may be less adherent to therapy due to OOP burden, suggesting a potential area of alignment for payer and manufacturer collaboration.
The distribution of DIR funds may create a perverse incentive for payers which favors high list price / high rebate drugs. Manufacturers must be cognizant of this fact as they engage in contract negotiations with Part D payers.


